Improvement in Glycaemic Control Following External Counter-pulsation (ECP) Therapy in Diet-Controlled Type 2 Diabetes: A Case Report
DOI:
https://doi.org/10.37934/jarsbs.39.1.227234Abstract
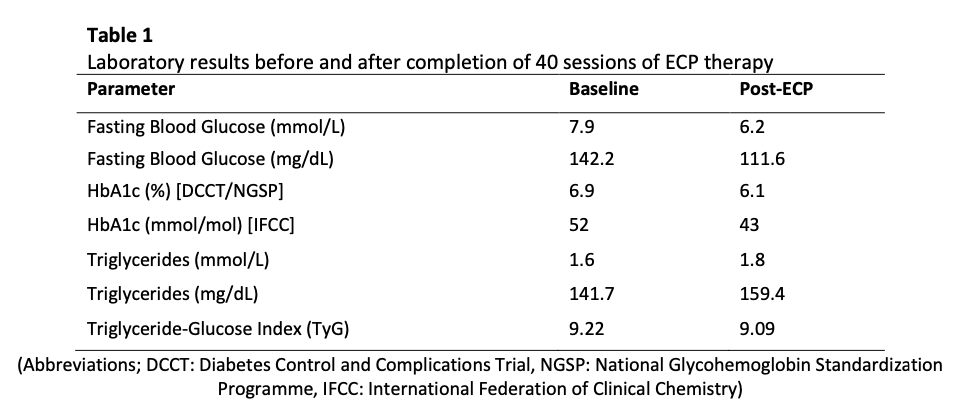
External Counter-pulsation (ECP) is an FDA-approved, non-invasive therapy primarily indicated for patients with refractory angina and selected cases of heart failure. ECP works by sequentially inflating and deflating pneumatic cuffs on the lower limbs, synchronised with the cardiac cycle, to augment diastolic coronary perfusion and reduce cardiac workload. Beyond its cardiovascular applications, emerging evidence suggests that ECP may exert favourable effects on metabolic parameters, including glycaemic control, through mechanisms such as improved peripheral circulation, enhanced endothelial function, and increased insulin sensitivity. However, data on its efficacy in patients with diet-controlled type 2 diabetes mellitus (T2DM) remain limited. We present the case of a 69-year-old Chinese female with a history of diet-controlled T2DM, who underwent 40 sessions of ECP therapy over a period of several weeks. During the intervention, no changes were made to her diet, physical activity level, or medication regimen. Pre- and post-intervention biochemical assessments demonstrated a reduction in fasting plasma glucose from 7.9 mmol/L (142.2 mg/dL) to 6.2 mmol/L (111.6 mg/dL). Glycated haemoglobin (HbA1C) decreased from 6.9% to 6.1%, indicating improved long-term glycaemic control. Furthermore, her Triglyceride-Glucose (TyG) index, a surrogate marker of insulin resistance, decreased from 9.22 to 9.09 despite a mild increase in serum triglycerides from 1.6 mmol/L (141.7 mg/dL) to 1.8 mmol/L (159.4 mg/dL). In addition to the objective biochemical improvements, the patient reported notable subjective benefits, including enhanced energy levels and improved overall well-being, without experiencing any adverse effects attributable to ECP. This case highlights the potential of ECP as an adjunctive intervention for metabolic optimisation in patients with T2DM, particularly those who are managed with lifestyle modification alone. While the observed improvements in glycaemic markers are encouraging, the single-patient nature of this report limits the applicability of the findings. Further controlled studies with larger sample sizes are warranted to elucidate the underlying mechanisms, determine the magnitude and durability of metabolic benefits, and assess the role of ECP in comprehensive diabetes management strategies. If substantiated, ECP may represent a novel, non-pharmacological option for enhancing glycaemic control in select patients with T2DM.