A Computational Study of Hospital Isolation Room Environment to Assess the Spread of Airborne Contaminants
DOI:
https://doi.org/10.37934/progee.31.1.116Keywords:
Hospital Isolation Room Environment, Air Borne Diseases, Ventilation, Air Change Per Hour, Computational Fluid DynamicsAbstract
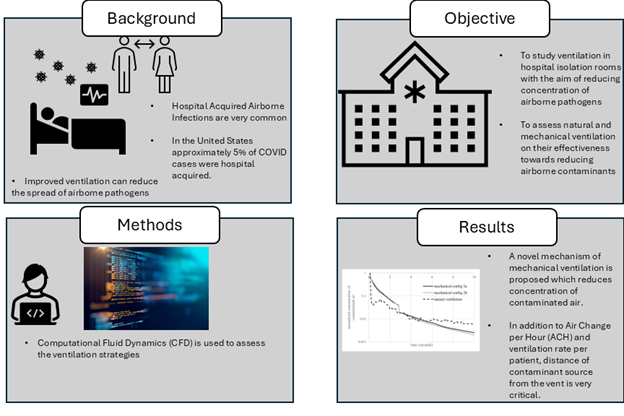
The safety of healthcare workers and patients in hospitals is a matter of paramount importance. Therefore, the significance of adequate ventilation in hospital rooms towards controlling airborne infections cannot be ignored. Although several reports discuss natural and mechanical ventilation in hospital isolation rooms, conflicting opinions recommend one ventilation method. There is also a paucity of information that relates engineering evaluation of hospital room ventilation to the design standards laid down by established public health agencies in the United States. This research aims to study hospital isolation room ventilation performance using natural and mechanical ventilation methods and assess certain guidelines on hospital room ventilation. Computational Fluid Dynamics is used to evaluate the concentration of contaminated air following a coughing event within a hospital isolation room using natural and mechanical ventilation. A novel technique employing a mechanical exhaust tube is proposed that may substantially reduce contaminant concentration. Within the same hospital isolation room, the normalized maximum concentration of contaminated air is much lower with two different mechanical ventilation methods (0.2% and 0.25%) than with the natural ventilation method (0.6%), suggesting that mechanical ventilation methods are more effective in reducing the concentration of contaminated air. In addition to established design parameters such as Air Change per Hour (ACH) and ventilation volume per patient, closer proximity to the vent from the contaminant source may also play a critical role in reducing contaminant concentration.
References
[1] J. Kutter, M. Spronken, P. Fraaij, R. Fouchier, and S. Herfst, Transmission Routes of Respiratory Viruses among Humans, Current Opinion in Virology. 28 (2018) 142–151. https://doi.org/10.1016/j.coviro.2018.01.001
[2] Our World in Data, Death Rate from Infectious Diseases, 2024. https://ourworldindata.org/grapher/infectious-disease-death-rates?tab=chart
[3] Center for Disease Control and Prevention. Respiratory Illnesses Data Channel, 2024. https://www.cdc.gov/respiratory-viruses/data/index.html
[4] World COVID-19 Dashboard, World Health Organization Data, 2024. https://data.who.int/dashboards/covid19/deaths?n=o (accessed 31 July 2024).
[5] K.M. Hatfield, J. Baggs, A. Maillis, S. Warner, J.A. Jernigan, S.S. Kadri, M. Klompas, and S. Reddy, Assessment of Hospital-Onset SARS-CoV-2 Infection Rates and Testing Practices in the US, 2020-2022, JAMA Network Open. 6.8 (2023) e2329441-e2329441. https://doi.org/10.1001/jamanetworkopen.2023.29441
[6] W.J. Kowalski. Air-Treatment Systems for Controlling Hospital-Acquired Infections. HPAC Engineering. 1 (2007) 2-22.
[7] A. Sikora, and F. Zahra, Nosocomial infections, StatPearls Publishing LLC, 2020.
[8] S.S. Magill, E. O’Leary, S. J. Janelle, D. L. Thompson, G. Dumyati, J. Nadle, ... J. R. Edwards, Emerging Infections Program Hospital Prevalence Survey Team. Changes in prevalence of health care-associated infections in US hospitals, The New England Journal of Medicine. 379.18 (2018) 1732-1744. https://doi.org/10.1056/NEJMoa1801550
[9] I. Eames, J.W. Tang, Y. Li, and P. Wilson, Airborne Transmission of Disease in Hospitals, Journal of the Royal Society Interface. 6 (2009) S697-S702. https://doi.org/10.1098/rsif.2009.0407.focus
[10] V.C. Cheng, K.S. Fung, G.K. Siu, S.C. Wong, L.S. Cheng, M.S. Wong, L.K. Lee, W.M. Chan, K.Y. Chau, J.S.L. Leung, A.W.H. Chu, Nosocomial Outbreak of Coronavirus Disease 2019 by Possible Airborne Transmission Leading to a Superspreading Event, Clinical Infectious Diseases. 73.6 (2021) e1356-e1364. https://doi.org/10.1093/cid/ciab313
[11] H. Helanne, E. Forsblom, K. Kainulainen, A. Jӓrvinen, and E. Kortela, Incidence and Outcome of Hospital-Acquired Covid-19 Infections in Secondary and Tertiary Care Hospitals in the Era of Covid-19 Vaccinations, Antimicrobial Stewardship & Healthcare Epidemiology. 3.1 (2023) e216. https://doi.org/10.1017/ash.2023.489
[12] A.R. Escombe, C.C. Oeser, R.H. Gilman, M. Navincopa, E. Ticona, W. Pan, C. Martinez, J. Chacaltana, R. Rodriguez, D.A. Moore, J.S. Friedland, and C.A. Evans, Natural Ventilation for the Prevention of Airborne Contagion, PLOS Medicine. 4.2 (2007) e68. https://doi.org/10.1371/journal.pmed.0040068
[13] N. Mingotti, D. Grogono, G. dello loio, M. Curran, K. Barbour, M. Taveira, J. Rudman, C. Haworth, R. Floto, and A. Woods, The Impact of Hospital-Ward Ventilation on Airborne-Pathogen Exposure, American Journal of Respiratory and Critical Care Medicine. 203.6 (2021) 766-769. https://doi.org/10.1164/rccm.202009-3634LE
[14] H. Qian, Y. Li, W.H. Seto, P. Ching, W.H. Ching, and H.Q. Sun, Natural ventilation for reducing airborne infection in hospitals, Building and Environment. 45.3 (2010) 559-565. https://doi.org/10.1016/j.buildenv.2009.07.011
[15] H.B. Awbi, Ventilation for Good Indoor Air Quality and Energy Efficiency, Energy. 112 (2017) 277-286. https://doi.org/10.1016/j.egypro.2017.03.1098
[16] J. Atkinson (Ed.), Y. Chartier, C.L. Pessoa-Silva, P. Jensen, Y. Li, and W.H. Seto, Natural Ventilation for Infection Control in Health-Care Settings, WHO Publication/Guidelines, Canberra, 2009.
[17] S. Bhattacharyya, K. Dey, A.R. Paul, R.A. Biswas, A Novel CFD Analysis to Minimize the Spread of COVID-19 Virus in Hospital Isolation Room, Chaos, Solitons & Fractals. 139 (2020) 110294. https://doi.org/10.1016/j.chaos.2020.110294
[18] C. Méndez, J.F. San José, J.M. Villafruela, and F. Castro, Optimization of a Hospital Room by means of CFD for More Efficient Ventilation, Energy and Buildings. 40.5 (2008) 849-854. https://doi.org/10.1016/j.enbuild.2007.06.003
[19] Chau, C.H. Liu, and M.K. Leung, CFD Analysis of the Performance of a Local Exhaust Ventilation System in a Hospital Ward, Indoor and Built Environment. 15.3 (2006) 257-271. https://doi.org/10.1177/1420326X06066123
[20] C.B. Beggs, K.G. Kerr, C.J. Noakes, E.A. Hathway, and P.A. Sleigh, The Ventilation of Multiple-Bed Hospital Wards: Review and Analysis, American Journal of Infection Control. 36.4 (2008) 250-259. https://doi.org/10.1016/j.ajic.2007.07.012
[21] W.Z. Lu, A.Y. Leung, S.H. Yan, and A.T.P. So, A Preliminary Parametric Study on Performance of Sars Virus Cleaner using CFD Simulation, International Journal for Numerical Methods in Fluids. 47 (2005) 1137-1146. https://doi.org/10.1002/fld.909
[22] R.E. Stockwell, E.L. Ballard, P. O'Rourke, L.D. Knibbs, L. Morawska, and S.C. Bell, Indoor Hospital Air and the Impact of Ventilation on Bioaerosols: A Systematic Review, Journal of Hospital Infection. 103.2 (2019) 175-184. https://doi.org/10.1016/j.jhin.2019.06.016
[23] F. Mills, Indoor Air Standards in Hospitals, Business Briefing: Hospital Engineering and Facilities Management. (2004) 43–46.
[24] A.R. Escombe, E. Ticona, V. Chávez-Pérez, M. Espinoza, and D.A. Moore, Improving Natural Ventilation in Hospital Waiting and Consulting Rooms to Reduce Nosocomial Tuberculosis Transmission Risk in A Low Resource Setting, BMC Infectious Diseases. 19 (2019) 1-7. https://doi.org/10.1186/s12879-019-3717-9
[25] ANSYS, Fluent 18 Manual, 2017.
[26] Q. Chen, Comparison of Different k-ε Models for Indoor Air Flow Computations, Numerical Heat Transfer, Part B, Fundamentals. 28.3 (1995) 353-369. https://doi.org/10.1080/10407799508928838
[27] J. Posner, C. Buchanan, and D. Dunn-Rankin, Measurement and Prediction of Indoor Air Flow in a Model Room, Energy and Buildings. 35.5 (2003) 515-526. https://doi.org/10.1016/S0378-7788(02)00163-9
[28] Z. Bolashikov, and A. Melikov, Methods for Cleaning and Protection of Building Occupants from Airborne Pathogens, Building and Environment. 44.7 (2009) 1378-1385. https://doi.org/10.1016/j.buildenv.2008.09.001
[29] S. Thool, S. Sinha, Performance Evaluation of Conventional Mixing Ventilation Systems for Operating Room in the view of Infection Control by Numerical Simulation, IJBSBT. 6.4 (2014) 87-98. http://dx.doi.org/10.14257/ijbsbt.2014.6.4.09
[30] W. Cao, B. Sun, Y. Zhao, Q. Shi, and Y. Wang, Study on the Transmission Route of Virus Aerosol Particles and Control Technology of Air Conditioning in the Enclosed Space, The European Physical Journal Plus. 136 (2021) 1-15. https://doi.org/10.1140/epjp/s13360-021-02058-8
[31] M. Alkhalaf, A. Ilinca, and M. Hayyani, CFD Investigation of Ventilation Strategies to Remove Contaminants from a Hospital Room, Design. 7.1 (2023) 5. https://doi.org/10.3390/designs7010005
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Progress in Energy and Environment

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.