Could Mobile Air Supply Unit Enhance Airflow Distribution in Office Environments?
DOI:
https://doi.org/10.37934/progee.31.1.1731Keywords:
Airflow Distribution, Office Environment, Air Supply Unit, Onsite Measurement, Numerical SimulationAbstract
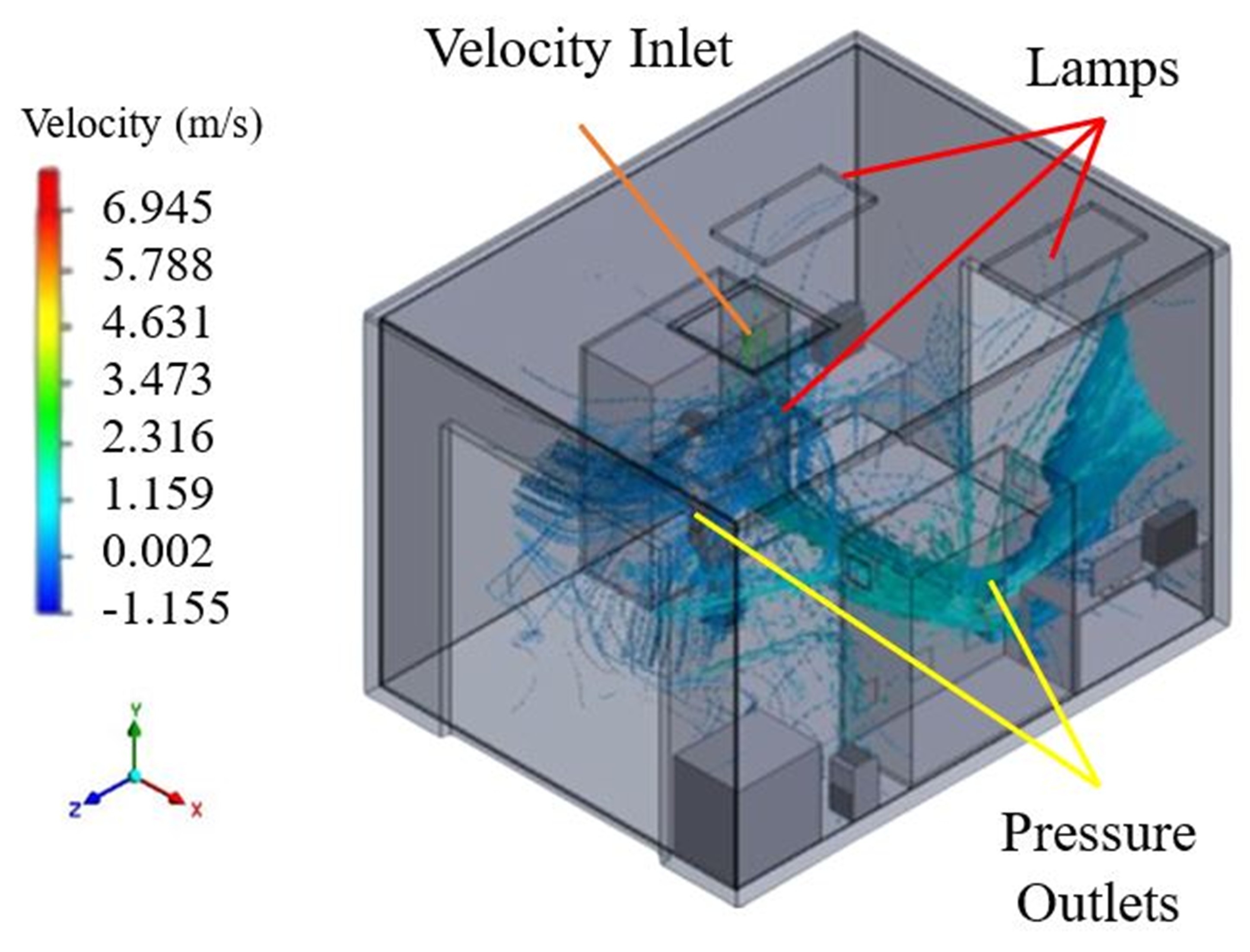
Effective airflow management in office settings is crucial for good indoor air quality and occupant comfort. Poor air circulation can lead to health issues like increased respiratory infections and decreased productivity. This study examines the effectiveness of mobile air supply (MAS) units in enhancing airflow distribution within an office, comparing them with a primary air-conditioning system. A computational fluid dynamics (CFD) simulation using the Renormalization Group (RNG) k-ε turbulence model based on Reynolds-Averaged Navier-Stokes equations predicted airflow distribution. The model showed high accuracy, with an average relative error of 6.6%. The installation locations of MAS units did not significantly affect airflow around occupants. While MAS units can locally enhance airflow, their overall effect on office air distribution is minimal compared to the primary air-conditioning system. The highest velocities were up to 3 m/s near workstations, which diluted particulates but also raised thermal discomfort concerns. Units placed behind obstacles like furniture showed poor air mixing and ineffective distribution. The study highlights the importance of strategically positioning MAS units to optimize air distribution without compromising comfort. Future research should explore particle dispersion within these configurations and extend the use of mobile units to various building types, aiming to improve indoor air quality across different environments. Such research would support adaptive ventilation strategies that enhance air quality and energy efficiency, aligning with the United Nations Sustainable Development Goal (SDG) 3: Good Health and Well-being.
References
[1] H. Tan, K.Y. Wong, M.H.D. Othman, H.Y. Kek, R.A. Wahab, G.K.P. Ern, W.T. Chong, and K.Q. Lee, Current and Potential Approaches on Assessing Airflow and Particle Dispersion in Healthcare Facilities: A Systematic Review. Environmental Science and Pollution Research 29 (2022) 80137-80160. https://doi.org/10.1007/s11356-022-23407-9
[2] W.H. Organization, Household Air Pollution, 2024.
[3] F.A. Rabi, M.S. Al Zoubi, G.A. Kasasbeh, D.M. Salameh, and A.D. Al-Nasser, SARS-CoV-2 and Coronavirus Disease 2019: What We Know So Far. Pathogens 9(3) (2020) 231. https://doi.org/10.3390/pathogens9030231
[4] D.R. Feikin, M.M. Higdon, L.J. Abu-Raddad, N. Andrews, R. Araos, Y. Goldberg, M.J. Groome, A. Huppert, K.L. O'Brien, and P.G. Smith, A. Wilder-Smith, S. Zeger, M. Deloria Knoll, M.K. Patel, Duration of Effectiveness of Vaccines against SARS-CoV-2 Infection and COVID-19 Disease: Results of a Systematic Review and Meta-Regression. The Lancet 399(10328) (2022) 924-944. https://doi.org/10.1016/S0140-6736(22)00152-0
[5] J.M. Samet, and J.D. Spengler, Indoor Environments and Health: Moving into the 21st Century. American Journal of Public Health 93 (9) (2003) 1489-1493. https://doi.org/10.2105/AJPH.93.9.1489
[6] G.E. Kaufman, and G. Griffith, Chapter 12 - Sustainable Practices for Zoological Veterinary Medicine, in: R.E. Miller, M. Fowler (Eds.) Fowler's Zoo and Wild Animal Medicine, W.B. Saunders, Saint Louis, 2012, pp. 86-97.
[7] A. Norhidayah, L. Chia-Kuang, M. Azhar, and S. Nurulwahida, Indoor Air Quality and Sick Building Syndrome in Three Selected Buildings. Procedia Engineering 53 (2013) 93-98. https://doi.org/10.1016/j.proeng.2013.02.014
[8] A. Singh, C.N. Kesavachandran, R. Kamal, V. Bihari, A. Ansari, P.A. Azeez, P.N. Saxena, A.K. Ks, and A.H. Khan, Indoor Air Pollution and its Association with Poor Lung Function, Microalbuminuria and Variations in Blood Pressure among Kitchen Workers in India: A Cross-Sectional Study. Environmental Health 16 (2017) 33. https://doi.org/10.1186/s12940-017-0243-3
[9] A. Peters, E. Liu, R.L. Verrier, J. Schwartz, D.R. Gold, M. Mittleman, J. Baliff, J.A. Oh, G. Allen, and K. Monahan, Air Pollution and Incidence of Cardiac Arrhythmia. Epidemiology 11(1) (2000) 11-17. https://doi.org/10.1097/00001648-200001000-00005
[10] J. Kim, and R. de Dear, Impact of Different Building Ventilation Modes on Occupant Expectations of the Main IEQ Factors. Building and Environment 57 (2012) 184-193. https://doi.org/10.1016/j.buildenv.2012.05.003
[11] D. Khovalyg, O.B. Kazanci, H. Halvorsen, I. Gundlach, W.P. Bahnfleth, J. Toftum, and B.W. Olesen, Critical Review of Standards for Indoor Thermal Environment and Air Quality. Energy and Buildings 213 (2020) 109819. https://doi.org/10.1016/j.enbuild.2020.109819
[12] P. Wargocki, Ventilation, Thermal Comfort, Health and Productivity, in: A Handbook of Sustainable Building Design and Engineering, Routledge, 2018, pp. 209-225.
[13] S. Dimitroulopoulou, M.R. Dudzińska, L. Gunnarsen, L. Hägerhed, H. Maula, R. Singh, O. Toyinbo, and U. Haverinen-Shaughnessy, Indoor Air Quality Guidelines from Across the World: An Appraisal Considering Energy Saving, Health, Productivity, and Comfort. Environment International 178 (2023) 108127. https://doi.org/10.1016/j.envint.2023.108127
[14] I.H. Hatif, H. Mohamed Kamar, N. Kamsah, K.Y. Wong, and H. Tan, Influence of Office Furniture on Exposure Risk to Respiratory Infection under Mixing and Displacement Air Distribution Systems. Building and Environment 239 (2023) 110292. https://doi.org/10.1016/j.buildenv.2023.110292
[15] Y. Katsumata, M. Sano, H. Okawara, T. Sawada, D. Nakashima, G. Ichihara, K. Fukuda, K. Sato, and E. Kobayashi, Laminar Flow Ventilation System to Prevent Airborne Infection during Exercise in the COVID-19 Crisis: A Single-Center Observational Study. PLoS One, 16(11) (2021) e0257549. https://doi.org/10.1371/journal.pone.0257549
[16] R. Cao, P. Qiu, B. Xu, J. Lin, D. Chu, and Z. Fan, Effectiveness of Interventions to Reduce Aerosol Generation in Dental Environments: A Systematic Review. Preventive Medicine Reports 35 (2023) 102383. https://doi.org/10.1016/j.pmedr.2023.102383
[17] N. Bergam, L. Chen, S. Lende, S. Snow, J. Zhang, M. DiBuono, and N. Calzaretto, Designing and Simulating a Smart Air Purifier to Combat HVAC-induced COVID-19 Transmission, in: 2020 IEEE MIT Undergraduate Research Technology Conference (URTC), 2020, pp. 1-5.
[18] C.-H. Huang, T. Bui, D. Hwang, J. Shirai, E. Austin, M. Cohen, T. Gould, T. Larson, I. Novosselov, S. Tan, J. Fox, and E. Seto, Assessing the Effectiveness of Portable HEPA Air Cleaners for Reducing Particulate Matter Exposure in King County, Washington Homeless Shelters: Implications for Community Congregate Settings. Science of The Total Environment 891 (2023) 164402. https://doi.org/10.1016/j.scitotenv.2023.164402
[19] B. Thottiyil Sultanmuhammed Abdul Khadar, J. Sim, J. McDonagh, V.M. McDonald, and B.G. Mitchell, Air Purifiers for Reducing the Incidence of Acute Respiratory Infections in Australian Residential Aged Care Facilities: A Study Protocol for a Randomised Control Trial. Infection, Disease & Health 28 (3) (2023) 239-245. https://doi.org/10.1016/j.idh.2023.05.006
[20] H.Y. Kek, H. Tan, M.H.D. Othman, W.T. Chong, B.B. Nyakuma, A. Bazgir, Y. Zhang, and K.Y. Wong, Is Thermal-Guided Mobile Air Supply a Practical Measure in Burn Isolation Wards? Potential Future Applications. Journal of Thermal Analysis and Calorimetry 149 (2024) 11205-11221. https://doi.org/10.1007/s10973-024-13045-3
[21] F. Timo, W. Felix, Z. Nicole, M. Nico, and K. Thomas, Effect of Portable HEPA Filters on COVID-19 Period Prevalence: An Observational Quasi-Interventional Study in German Kindergartens. BMJ Open 13(7) (2023) e072284. https://doi.org/10.1136/bmjopen-2023-072284
[22] C.M. Walker, and G. Ko, Effect of Ultraviolet Germicidal Irradiation on Viral Aerosols. Environmental Science & Technology 41(15) (2007) 5460-5465. https://doi.org/10.1021/es070056u
[23] A. Abbaspour, A. Bahadori-Jahromi, A. Janbey, P.B. Godfrey, and S. Amirkhani, Enhancing Indoor Air Quality and Regulatory Compliance: An In-Depth Comparative Study on Ventilation Strategies and their Impact on SARS-CoV-2 Transmission Risk. Sustainability 16(1) (2023) 271. https://doi.org/10.3390/su16010271
[24] H.C. Burridge, S. Liu, S. Mohamed, S.G.A. Wood, and C.J. Noakes, Coupled Indoor Air Quality and Dynamic Thermal Modelling to Assess the Potential Impacts of Standalone HEPA Filter Units in Classrooms. Indoor Environments 1(3) (2024) 100034. https://doi.org/10.1016/j.indenv.2024.100034
[25] A.C. von Vogelsang, P. Förander, M. Arvidsson, and P. Löwenhielm, Effect of Mobile Laminar Airflow Units on Airborne Bacterial Contamination during Neurosurgical Procedures. Journal of Hospital Infection 99(3) (2018) 271-278. https://doi.org/10.1016/j.jhin.2018.03.024
[26] S.D. Lowther, W. Deng, Z. Fang, D. Booker, D.J. Whyatt, O. Wild, X. Wang, and K.C. Jones, How Efficiently can HEPA Purifiers Remove Priority Fine and Ultrafine Particles from Indoor Air?, Environment International 144 (2020) 106001. https://doi.org/10.1016/j.envint.2020.106001
[27] C. Wang, S. Holmberg, and S. Sadrizadeh, Numerical Study of Temperature-Controlled Airflow in Comparison with Turbulent Mixing and Laminar Airflow for Operating Room Ventilation. Building and Environment 144 (2018) 45-56. https://doi.org/10.1016/j.buildenv.2018.08.010
[28] C. Ren, H.-C. Zhu, and S.-J. Cao, Ventilation Strategies for Mitigation of Infection Disease Transmission in an Indoor Environment: A Case Study in Office. Buildings 12(2) (2022) 180. https://doi.org/10.3390/buildings12020180
[29] H. Tan, K.Y. Wong, M.H. Dzarfan Othman, H.Y. Kek, W.Y. Tey, B.B. Nyakuma, G.R. Mong, G. Kuan, W.S. Ho, H.S. Kang, D.D. Chin Vui Sheng, and R.A. Wahab, Controlling infectious airborne particle dispersion during surgical procedures: Why mobile air supply units matter?, Building and Environment, 223 (2022) 109489. https://doi.org/10.1016/j.buildenv.2022.109489
[30] J. Chen, and G. Tang, A Big-data Inspired Precision Improvement Algorithm for Autonomous Navigation Based on Period Variable Stars. Journal of Signal Processing Systems 93(7) (2021) 719-731. https://doi.org/10.1007/s11265-021-01639-1
[31] K.Y. Wong, H. Tan, B.B. Nyakuma, H.M. Kamar, W.Y. Tey, H. Hashim, M.C. Chiong, S.L. Wong, R.A. Wahab, G.R. Mong, W.S. Ho, M.H.D. Othman, and G. Kuan, Effects of Medical Staff’s Turning Movement on Dispersion of Airborne Particles under Large Air Supply Diffuser during Operative Surgeries. Environmental Science and Pollution Research 29(54) (2022) 82492-82511. https://doi.org/10.1007/s11356-022-21579-y
[32] M. Ahsan, Numerical Analysis of Friction Factor for A Fully Developed Turbulent Flow using k–ε Turbulence Model with Enhanced Wall Treatment. Beni-Suef University Journal of Basic and Applied Sciences 3(4) (2014) 269-277. https://doi.org/10.1016/j.bjbas.2014.12.001
[33] M. Lee, G. Park, C. Park, and C. Kim, Improvement of Grid Independence Test for Computational Fluid Dynamics Model of Building Based on Grid Resolution. Advances in Civil Engineering 2020 (2020) 8827936. https://doi.org/10.1155/2020/8827936
[34] R. Kumar A, K.C.K. Vijayakumar, and P. Srinivasan, Numerical Investigation of Heat Transfer across PVC Pipe Implanted RCC Roof for Thermal Comfort. International Journal of Applied Engineering Research 9 (2014) 26243-26258.
[35] H. Tan, K.Y. Wong, M.H.D. Othman, H.Y. Kek, B.B. Nyakuma, W.S. Ho, H. Hashim, R.A. Wahab, D.D.C.V. Sheng, N.H.A. Wahab, and A.S. Yatim, Why Do Ventilation Strategies Matter in Controlling Infectious Airborne Particles? A Comprehensive Numerical Analysis in Isolation Ward. Building and Environment 231 (2023) 110048. https://doi.org/10.1016/j.buildenv.2023.110048
[36] S. Sadrizadeh, S. Holmberg, and P.V. Nielsen, Three Distinct Surgical Clothing Systems in a Turbulent Mixing Operating Room Equipped with Mobile Ultraclean Laminar Airflow Screen: A Numerical Evaluation. Science and Technology for the Built Environment 22(3) (2016) 337-345. https://doi.org/10.1080/23744731.2015.1113838
[37] B. Griefahn, C. Künemund, and U. Gehring, The Significance of Air Velocity and Turbulence Intensity for Responses to Horizontal Drafts in a Constant Air Temperature of 23C. International Journal of Industrial Ergonomics 26 (6) (2000) 639-649. https://doi.org/10.1016/S0169-8141(00)00033-0
[38] K.Y. Wong, M.K. Haslinda, K. Nazri, and S.N. Alia, Effects of Surgical Staff Turning Motion on Airflow Distribution Inside a Hospital Operating Room. Evergreen 6(1) (2019) 52-58.
[39] U. Manual, ANSYS FLUENT 12.0, Theory Guide, 67 (2009).
[40] K. Wong, H. Kamar, and N. Kamsah, Enhancement of Airborne Particles Removal in a Hospital Operating Room. International Journal of Automotive and Mechanical Engineering 16(4) (2019) 7447-7463. https://doi.org/10.15282/ijame.16.4.2019.17.0551
[41] H.M. Kamar, N. Kamsah, K.Y. Wong, M.N. Musa, and M.S. Deris, Field Measurement of Airborne Particulate Matters Concentration in a Hospital's Operating Room. Jurnal Teknologi (Science & Engineering) 77(30) (2015) 63-67. https://doi.org/10.11113/jt.v77.6869
[42] I.S.O. Standard, ISO 14644-1, Cleanrooms and associated controlled environments, in: Classification of air cleanliness, Institute of Environmental Sciences and Technology, United Kingdom, 1999.
[43] H. Tan, M.H.D. Othman, H.Y. Kek, W.T. Chong, S.L. Wong, G.K.P. Ern, G.R. Mong, W.S. Ho, P.C. Leng, M.N.H. Mat, and K. Wong, Would Sneezing Increase the Risk of Passengers Contracting Airborne Infection? A Validated Numerical Assessment in a Public Elevator. Energy and Buildings 297 (2023) 113439. https://doi.org/10.1016/j.enbuild.2023.113439
[44] K.Y. Wong, H. Tan, B.B. Nyakuma, H.M. Kamar, W.Y. Tey, H. Hashim, M.C. Chiong, S.L. Wong, R.A. Wahab, G.R. Mong, W.S. Ho, M.H.D. Othman, and G. Kuan, Effects of Medical Staff’s Turning Movement on Dispersion of Airborne Particles under Large Air Supply Diffuser During Operative Surgeries. Environmental Science and Pollution Research 29 (2022) 82492-82511. https://doi.org/10.1007/s11356-022-21579-y
[45] F. Cheng, Y. Cheng, Z. Lin, Experimental Study of Draft-Related Local Discomfort in a Room with Stratum Ventilation. Applied Thermal Engineering 234 (2023) 121259. https://doi.org/10.1016/j.applthermaleng.2023.121259
[46] I.H. Hatif, H. Mohamed Kamar, N. Kamsah, K.Y. Wong, and H. Tan, Influence of Office Furniture on Exposure Risk to Respiratory Infection under Mixing and Displacement Air Distribution Systems. Building and Environment 239 (2023) 110292. https://doi.org/10.1016/j.buildenv.2023.110292
[47] H. Tan, K.Y. Wong, C.T. Lee, S.L. Wong, B.B. Nyakuma, R.A. Wahab, K.Q. Lee, M.C. Chiong, W.S. Ho, M.H.D. Othman, Y.H. Yau, H.Y. Kek, and H.M. Kamar, Numerical Assessment of Ceiling-Mounted Air Curtain on The Particle Distribution in Surgical Zone. Journal of Thermal Analysis and Calorimetry 148 (2022) 3005-3018. https://doi.org/10.1007/s10973-022-11466-6
[48] K. Wong, H. Kamar, and N. Kamsah, Medical Staff’s Posture on Airflow Distribution and Particle Concentration in an Operating Room, in: IOP Conference Series: Materials Science and Engineering, IOP Publishing, 2020, pp. 012103.
[49] H. Tan, K.Y. Wong, M.H.D. Othman, B.B. Nyakuma, D.D.C. Vui Sheng, H.Y. Kek, W.S. Ho, H. Hashim, M.C. Chiong, M.A. Zubir, N.H. Abdul Wahab, S.L. Wong, R. Abdul Wahab, and I.H. Hatif, Does Human Movement-Induced Airflow Elevate Infection Risk in Burn Patient’s Isolation Ward? A Validated Dynamics Numerical Simulation Approach. Energy and Buildings 283 (2023) 112810. https://doi.org/10.1016/j.enbuild.2023.112810
[50] H.M. Kamar, K.Y. Wong, and N. Kamsah, The Effects of Medical Staff Turning Movements on Airflow Distribution and Particle Concentration in an Operating Room. Journal of Building Performance Simulation 13(6) (2020) 684-706. https://doi.org/10.1080/19401493.2020.1812722
[51] H.Y. Kek, H. Tan, M.H.D. Othman, B.B. Nyakuma, P.S. Goh, S.L. Wong, X. Deng, P.C. Leng, A.S. Yatim, and K.Y. Wong, Perspectives on Human Movement Considerations in Indoor Airflow Assessment: A Comprehensive Data-Driven Systematic Review. Environmental Science and Pollution Research 30(58) (2023) 121253-121268. https://doi.org/10.1007/s11356-023-30912-y
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Progress in Energy and Environment

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.